What problems does COVID-19 present for pregnant women, especially in hotspots?
There are many unanswered questions about COVID-19 and how it may impact pregnant women and their babies. We currently do not know if pregnant women are more likely to have more serious COVID-19 symptoms as compared to non-pregnant members of the public. However, we do know the risk of some respiratory infections may increase during pregnancy. In our previous experience with other respiratory viruses such as Influenza and SARS-CoV, we see that pregnancy increases the risk of infection and of severe illness due to a lowered immune state. Based on the historically greater risk for other respiratory infections, pregnant women should be considered as an at-risk population for COVID-19. Dr. Kathleen Horowitz, MEDNAX’s National Clinical Director HRO for Labor and Delivery, states that, “from a pregnancy standpoint, it was thought that pregnant women would do worse with this respiratory illness. The good news is that the data so far around COVID-19 shows that pregnant women behave like the general population, which is great news for our moms.” In a recent study of 43 COVID-19-positive pregnant women identified over a two-week period in two New York City Hospitals, it was found that 86% showed symptoms associated with mild infection, 9.3% experienced a severe infection, and only 4.7% were in critical condition. This appears similar to what is described in the literature for non-pregnant people.[1]
Like non-pregnant patients, the predominant features of COVID-19 in pregnancy are fever, dry cough, and myalgia. However, in this same study of 43 COVID-19-positive pregnant women, a surprising number of women tested COVID-19 positive who did not present with symptoms at the time of labor and delivery. According to one study, “14 of 43 women in the case report were found to be COVID-19 positive despite having no symptoms at time of admission” (Breslin, 2020). This study supports the universal testing of pregnant women being admitted to the Labor & Delivery Unit. Because the transmission of the virus can occur before the presentation of symptoms, knowledge of COVID status can help our labor and delivery units to appropriately treat positive patients, conserve PPE and minimize risk of exposure of staff members. Knowledge of maternal COVID-19 status can also help guide our NICU colleagues in caring for newborn babies and minimizing the risk of transmission to this vulnerable population.
Recommendations / What are we doing to manage COVID-19 OB patients?
The World Health Organization (WHO) has established guidelines for maternal-fetal medicine (MFM) practitioners to: (1) reduce patient risk through healthcare exposure, and (2) to reduce the public health burden of COVID-19 transmission throughout the general population.
Pregnant women should be monitored for fever and symptoms of a respiratory infection. Initial screening should occur via phone call, or telehealth prior to an on-site visit. Patients should be instructed what to do if they have been exposed or demonstrate fever or respiratory symptoms.
Use of Personal Protective Equipment (PPE):
Dr. Brian Gilpin, National Clinical Director of OB Hospitalists at MEDNAX, noted that The Society of OBGYN Hospitalists recommends masking everyone. Dr. Gilpin stated, “I have seen in the press that ACOG and other organizations have asked the CDC to make a statement about COVID-19 and OB care, as there is some evidence that during the second stage of labor, where a woman is pushing, transmission is an aerosolized event. Much of the currently available literature includes data from New York, as it is one of the hardest-hit areas.”
National organizations vary in their recommendations on the use of N95 masks for healthcare personnel caring for women in the second stage of labor. Although there are certain procedures that meet the criteria for generating high concentrations of aerosols, the CDC states that data are limited on forceful exhalation during the second stage of labor. Proponents of universal masking point out that healthcare personnel caring for women in the second stage of labor are in close contact for long periods of time to provide support for breathing and pushing potentially increasing their risk of exposure to the virus.
The Association of Women’s Health, Obstetric and Neonatal Nurses (AWHONN) recommends all healthcare personnel wear appropriate PPE during the second stage of labor, including use of N95 masks when caring for women who are known or person under investigation (PUI) for COVID-19. Until universal testing is available, healthcare personnel should use N95 masks when caring for all women in the second stage of labor.[2]
Reducing the Risk of Transmission
Preventing COVID-19 exposure should be the priority for all pregnant women and healthcare personnel caring for pregnant women. All obstetrical visits should be completed using a telehealth mechanism unless an urgent problem warrants an in-person visit. Any elective or non-urgent visits should be postponed, or completed via telehealth approaches.
Visitor policies should be drafted for both outpatient office visits and hospital admission. Office visits should be limited to the patient only. One companion may accompany the patient during labor and delivery.
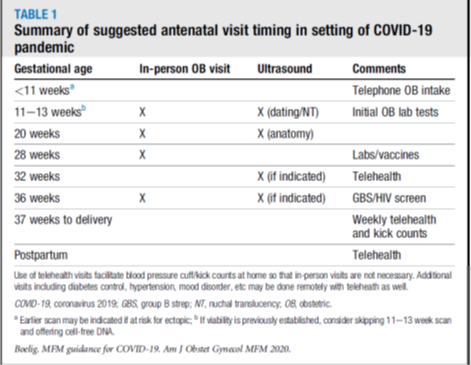
Table 1: Summary of suggested antenatal visit timing in setting of COVID-19 pandemic. Additional visits including follow up of diabetes control, hypertension, mood disorder etc. may be done remotely with telehealth.[3]
Recommendations for modified obstetric ultrasound timing are designed to limit the amount of face-to-face time, thus reducing the amount of exposure for both the patient and healthcare provider. In most cases, ultrasound findings may be reviewed with the patient using a telehealth mechanism.
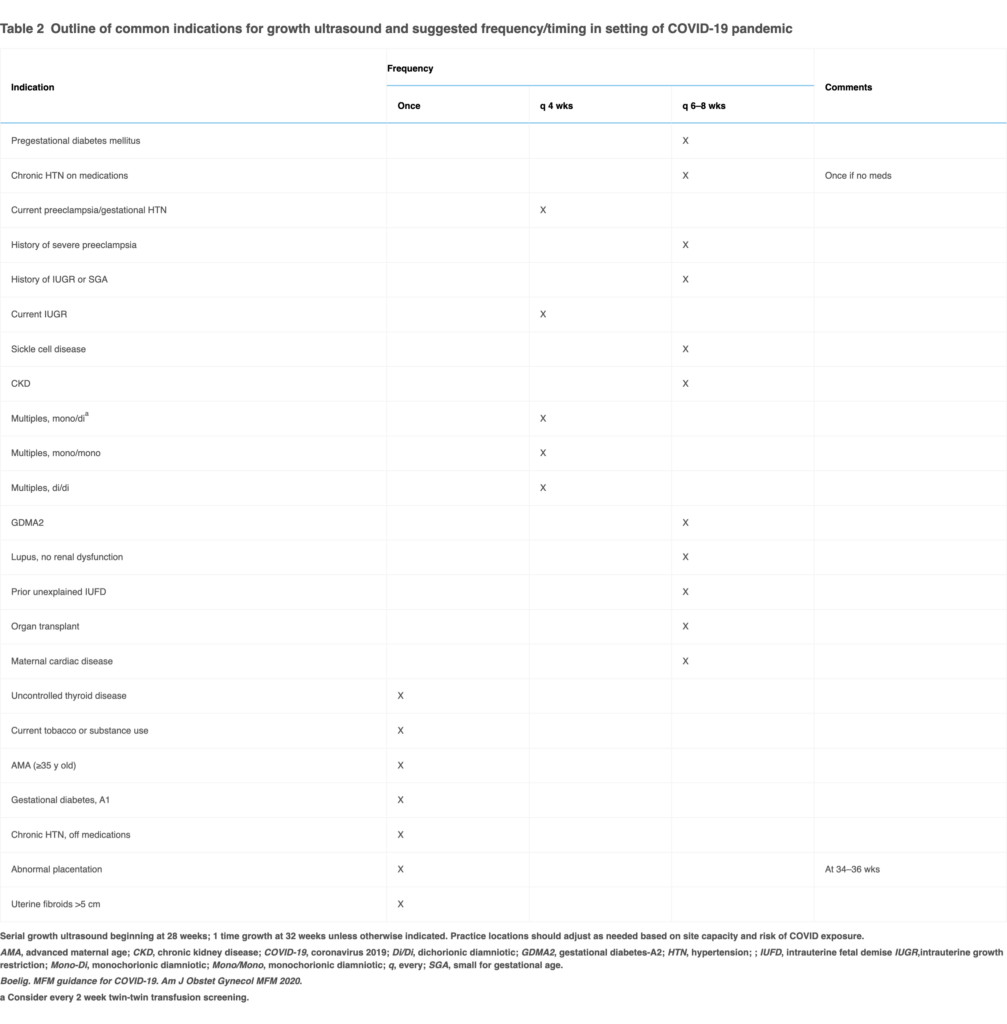 Table 2: Outline of common indications for growth ultrasound and suggested frequency/timing in setting of COVID-19 pandemic. Practice locations should adjust as needed based on site capacity and risk of COVID exposure.[4]
Table 2: Outline of common indications for growth ultrasound and suggested frequency/timing in setting of COVID-19 pandemic. Practice locations should adjust as needed based on site capacity and risk of COVID exposure.[4]
COVID-19 Screening/Testing
Numerous professional organizations and CMS agree that all patients must be screened for potential symptoms of COVID-19 prior to entering a healthcare facility, and staff must be routinely screened for symptoms or exposure. When adequate testing capability is established, patients should be screened by laboratory test before care, and staff working in these facilities should be regularly screened by laboratory test as well.[5] In addition, The Society for Obstetric Anesthesia and Perinatology (SOAP) recommends screening not only for the patient, but also screening the planned companion.[6]
Several facilities are establishing guidelines that include testing of every OB patient admitted into the hospital. Dr. Horowitz of Honor Health Medical System in Scottsdale, Arizona noted that they “started testing every patient admitted to their labor and delivery unit on April 20, 2020.” Dr. Horowitz notes further that “some patients with scheduled C-Sections and scheduled inductions in Washington state are being told to receive a COVID-19 test as an outpatient and based on the outcome of the test, OB/GYNs may recommend that they delay their scheduled procedures.”
What’s next? How do we recover from the pandemic?
How do we deal with that aftermath of COVID-19? Can we get back to what used to normal, or can we even get to a place that is better than before? Dr. Gilpin believes that “if we can enhance L&D processes in hospitals after COVID-19, it can help get hospitals back on their feet.”
Collecting information from OB hospitalist groups to obtain data around how COVID-19 is impacting their OB patients will help answer key questions and also help to establish definitive COVID-19 treatment plans.
Establishing clear and defined guidelines to move pregnant patients safely throughout their continuum of care will improve hospital efficiency and patient satisfaction. Timely transfer of documentation between providers and healthcare facilities including history and physical, laboratory, and radiology results. Healthcare providers must collaborate to streamline the antepartum, intrapartum, and postpartum periods for their patients. Surgical Directions offers an OB optimization program with solutions to improve throughput, patient preparation, staffing, provider satisfaction, and nursing proficiencies. This strategy provides hospitals with solutions to enhance predictability for efficiency, safety and the best quality care for pregnant patients.
There are several specific reasons why pregnant women and their health care providers may be uniquely affected by the COVID-19 pandemic. Due to the time-limited nature of pregnancy, safeguarding the fetus and managing the needs of a pregnant woman during the COVID-19 pandemic is fundamental for healthcare providers. The need for ongoing care and inability to completely avoid clinic and hospital settings because of need for fetal assessments and management of labor present some unique challenges that are not present in other medical disciplines. Surgical Directions, with their wealth and breadth of experience, is well-positioned to help healthcare facilities navigate these challenges.
For more information click on the contact button below.
[1] Noelle Breslin1, C. B.-B. (2020). COVID-19 infection among asymptomatic and symptomatic pregnant women: Two weeks of confirmed presentations to an affiliated pair of New York City hospitals. New York: Columbia University Medical Center.
[2] AWHONN. (2020, April 20). AWHONN COVID-19 Practice Guidance. Retrieved from Association of Women’s Health, Obstetric and Neonatal Nurses: https://awhonn.org/novel-coronavirus-covid-19/covid19-practice-guidance/
[3] Rupsa C. and Boelig, M. M. (2020). MFM Guidance for COVID-19. American Journal of Obstetrics & Gynecology MFM, doi: https://doi.org/10.1016/.
[4] Ibid.
[5] CMS. (2020). Opening Up America Again: CMS Recommendations Re-opening Facilities to Provide Non-emergent Non-COVID-19 Healthcare: Phase 1. Washington, DC: CMS.
[6] Society for Obstetric Anesthesia and Perinatology. (2020, April 10). Interim Considerations for Obstetric Anesthesia Care Related to COVID-19. Retrieved from SOAP: https://soap.org/education/provider-education/expert-summaries/interim-considerations-for-obstetric-anesthesia-care-related-to-covid19/



