Executive Summary
How Implementing the 3-Business Day Rule Improves Your Elective Summary Process
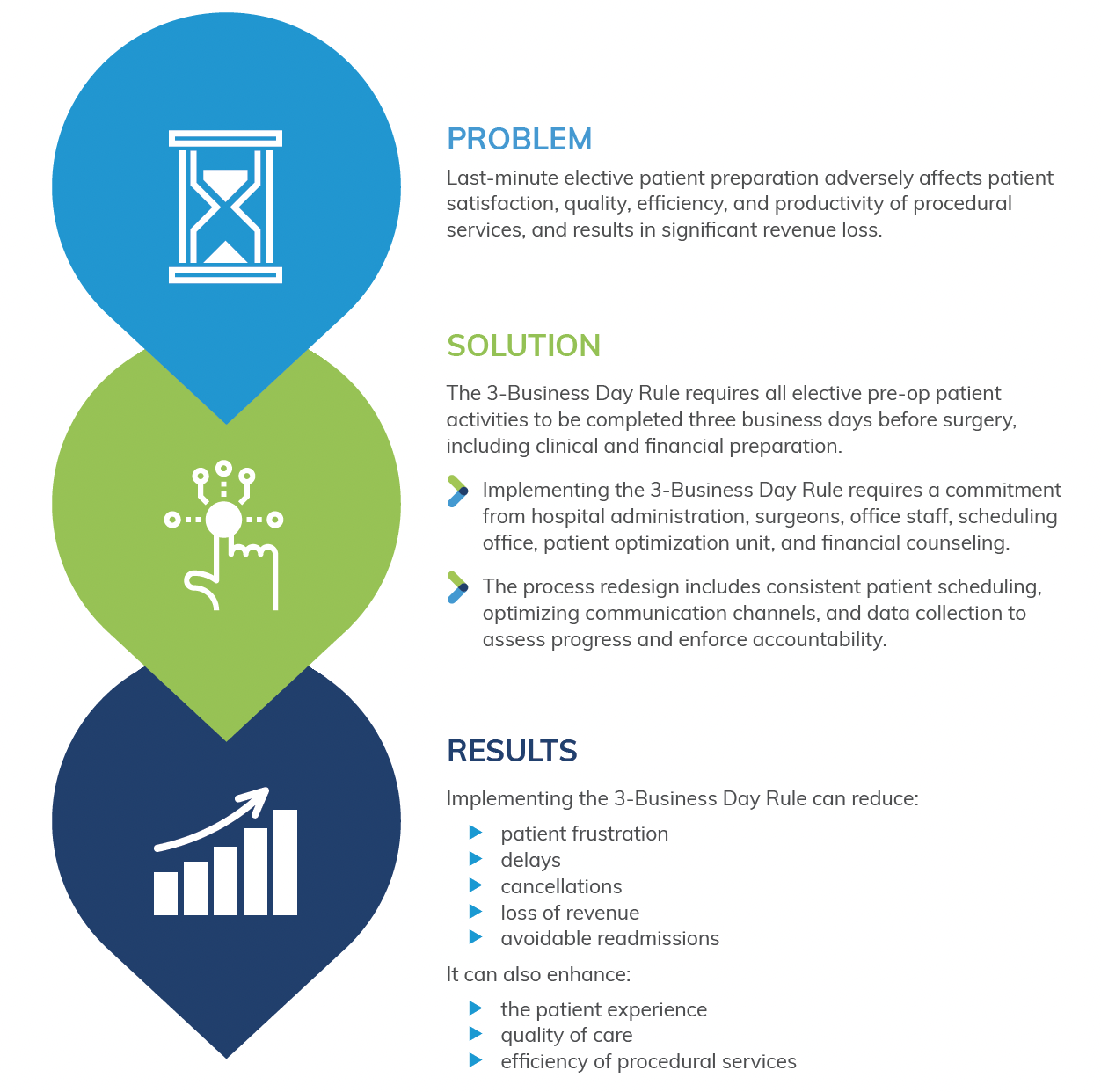
Unfortunately, elective surgery in the US is often an eleventh-hour effort. Either last-minute surgeon scheduling or hospitals that delay elective patient prep until a few days before surgery have become a major problem in elective procedural care. Last-minute elective patient preparation leads to patient frustration and confusion, delays, cancellations, loss of revenue, excessive length of stays, and avoidable readmissions. In a large and quantifiable way, this adversely affects the patient satisfaction, quality, efficiency, and productivity of your procedural services, as well as significant loss of revenue. Also, last-minute elective patient preparation places added burden on the units and personnel already in the midst of preparing more urgent cases for the operative schedule and a strained workforce as a result of national nursing shortages. With most elective surgery in the US scheduled at least 2-weeks prior to the day of surgery (Surgical Directions internal data) there is ample opportunity for a timely elective patient preparation process. In other words, the earlier patient preparation starts the better, and this includes both clinical optimization and financial preparation. To address these issues, Surgical Directions has reached consensus that a different and more consistent approach is required for the elective surgical patient. We call it the 3-Business Day Rule.
This simple rule states that all elective pre-op patient activity, including chart preparation and financial counseling/pre-authorization are complete at least 3 business days prior to the date of surgery. If not, the elective patient’s case is delayed until complete. Although a simple rule, it requires commitment from both the hospital’s administration, surgeons and office staff. Additionally, implementing accountability for the 3-Business Day Rule rule typically requires extensive redesign of pre-operative elective patient preparation process.
Implementing the 3-Business Day Rule requires working with appropriate constituents and accountability:
- Hospital senior administration. The single most important element in implementing the 3- Business Day Rule requires commitment of senior hospital administration. This commitment is based upon a detailed understanding of current quality issues, inefficiencies, productivity problems, and financial concerns related to last-minute elective patient scheduling. The hospital’s senior administration is also required to help enforce the new system and process.
- Surgeons’ offices. Implementing the 3-Business Day Rule requires working closely with both surgeons and their office staff. Bringing office staff into process re-design is recommended, as well as having townhall discussions during the redesign and implementation phase. Working with surgeons usually requires developing a joint steering committee that has access to baseline and ongoing analytics associated with benchmark goals.
- Scheduling Office. A consistent approach to both the timing and standardization of patient scheduling process is a crucial part of this redesign. Specifically, the boarding process should include all the appropriate information that expedites a seamless and timely elective patient pre-op process. At the time of scheduling both the patient optimization unit and the admitting office should be notified and receive patient contact information.
- Patient Optimization Unit. This unit must receive patient contact information as soon as the elective patient is scheduled for surgery. Surgical Directions has tried a variety of methods for two-way patient communication, but by far the best approach is hospital-based two-way EMR generated communicated or HIPAA compliant texting. This allows for optimum patient communication, minimizing the common practice of trying to reach patients by phone. It is also recommended in the initial scheduling process that the surgeon signs a scheduling form and checks a box permitting patient optimization to be guided by the anesthesia department’s protocols, guidelines and algorithms. We also recommend that most of patient optimization, including ROS reason of surgery, pertinent nursing information, prior surgeries, allergies, and current medications be obtained virtually by nurse-patient phone discussions. Optimally, either a pre-anesthesia testing RN or an advanced care provider conducts the chart review and enter orders for the appropriate labs, ECG, consults, etc., based on anesthesiology pre-surgical testing protocols.
- Patient Pre-Authorization and Financial Counseling. Pre-procedural elective patient financial counseling and insurance authorization—for both the surgeon and hospital—can be a time-consuming process. Much like patient clinical optimization, the financial encounter process should begin at the time at the time of scheduling, hopefully at least 5- 7 days prior to surgery. The admitting office should keep the surgeon and his office updated on the progress of obtaining authorizations. At three business days prior to surgery, if pre-authorization has not been obtained, a decision should be made to delay/ surgery.
- Improved two-way patient communications. As stated above, optimal two-way patient communication should ideally be EMR texting based. Traditional phone-based contact is typically fraught with lots of down time that includes unproductive phone tag and wasteful use of licensed RNs. Many hospitals already have texting systems that can be added to pre-op process for both clinical and financial communications.
- Data-collection, metrics, benchmarking. Implementing the 3-Business Day Rule requires data collection that includes in-depth analytics and benchmarking. This data should be used by the governing body to govern the process, assess progress, and manage accountability. Data collection should include chart completion (missing element tracker), pre-authorization completion, delays, cancellations, patient satisfaction, etc.
- Accountability and enforcement. Implementing the 3-Business Day Rule requires a leadership group that includes representatives from all those areas and clinicians involved in this process. It is particularly important that senior hospital administration give this group the authority to manage the process and implement accountability using data as appropriate. Representatives of this group should include surgeons, surgeon office personnel, admitting, anesthesiology, patient optimization unit, nursing leadership, and the administration.
Implementing timely elective patient optimization will reduce waste and confusion. An additional benefit of this process is the potential to receive revenue that is often not collected. Outside the 3-day window hospital-based patient workups can receive significant CPT-based revenue that would be precluded with the CMS 72-hour rule. This rule requires that all outpatient diagnostic or some other medical services delivered within 72 hours of hospital admission be bundled and billed collectively rather than individually. Components of this process should also include two-way text messaging and whenever possible virtual and continuous contact with the patient right up until the day of surgery. In conclusion, through mindful choreography,
the 3-Business Day Rule can improve patient optimization and preparation for surgery, improve case delays or cancellations, and improve financial revenue and significantly reduce cost for hospitals.
This simple rule requires completing all elective pre-op patient activity, including chart preparation and financial counseling/authorization, at least 3 business days prior to the date of surgery. If not, the elective patient’s case is delayed until complete. The implementation of this rule requires commitment from hospital administration, surgeons, and their office staff. The process redesign involves:
- Scheduling office
- Patient optimization unit
- Patient pre-authorization
- Financial counseling
- Improved two-way patient communications
Data collection, metrics, benchmarking, accountability, and enforcement are also crucial in this process. By implementing this rule, hospitals can improve patient experience, reduce cancellations, delays, and readmissions, and optimize revenue. It also reduces the burden on the workforce, especially in the context of the national nursing shortages. The hospital administration should work closely with surgeons, office staff, and other constituents to develop a detailed understanding of the current quality issues, inefficiencies, productivity problems, and financial concerns related to last-minute elective patient scheduling. With the right team and processes in place, hospitals can ensure that the elective surgery process runs smoothly and efficiently, resulting in better outcomes for patients and healthcare providers alike.



